Intro
The ways of healthcare payment are rapidly evolving. **Fee for Service Vs Value-based Care**models are reshaping how providers deliver care and how they’re paid. Traditional Fee-for-Service models reward providers for each test, procedure, or visit, without regard for patient outcomes. Value-based care reverses this trend, whereby the providers are rewarded based on how they ensure the patient is healthy and how they produce improved health outcomes.
Providers are now reimbursed based on patient outcomes, care quality, and cost efficiency. This change influences day-to-day activities, employee operations, investment in technology, and the relationship with patients. Understanding these changes helps providers plan for new payment models without financial strain.

How Fee-for-Service Models Compensate Providers
Under Fee-for-Service, providers are paid for every service delivered, including consultations, tests, procedures, and hospital visits. The payments are made regardless of whether they help in improving the health of patients or preventing complications in the long run. Revenue generation focuses entirely on service volume rather than health outcomes.
Revenue Structure Under Fee-for-Service
Providers increase revenue by delivering a higher volume of services. A greater number of visits by patients, more diagnostic tests, and more procedures increase the income. Each service has a fixed reimbursement rate. Payment occurs after service delivery and claim submission. Revenue correlates directly with patient volume.
This compensation model will motivate the providers to treat more patients within the same time slot. Preventive care and follow-ups carry no financial incentives. The financial risk to the providers of the patients is low. Administrative teams focus on accurate coding and timely claim submission to maximize reimbursement.
What Value-Based Care Means for Provider Reimbursement
Value-based care links physician payments to patient outcomes, care quality, and overall cost efficiency. Bonuses to the providers are based on quality standards, and fines for failure to achieve goals. This paradigm shift transforms healthcare into an outcome-based payment system as opposed to a volume-based payment system.
New Payment Structures Providers Face
The_ value-based care vs fee-for-service _comparison reveals fundamental changes in how providers earn income:
| Payment Model | Reimbursement Basis | Financial Risk |
| Fee-for-Service | Service volume | Low provider risk |
| Value-Based Care | Quality outcomes | Shared risk model |
| Bundled Payments | Episode of care | High provider risk |
Providers must track quality metrics, patient satisfaction scores, and cost efficiency. Compensation depends on meeting performance benchmarks across multiple categories. Payers establish quality thresholds that determine bonus payments or penalties.
Understanding Shared Savings Programs
Shared savings programs reward providers for reducing healthcare costs while maintaining quality. Insurers that maintain healthy patients and prevent unnecessary hospitalization share the cost savings. These programs require sophisticated tracking of patient populations and the total cost of care.
Why Providers Must Change Clinical Workflows
Value-based care requires providers to rethink how they deliver patient care. Older workflows built for high patient volumes don’t align with value-based care’s focus on quality and outcomes. The providers must have holistic solutions that focus on prevention and coordination.
Daily Operations That Need Adjustment
Providers need longer appointment times to properly assess patients. Coordinating care helps manage chronic conditions and prevent complications. Long patient visits enable the evaluation of health comprehensively. Regular follow-up calls monitor chronic conditions between visits.
Key workflow changes include:
- Care team meetings to coordinate treatment plans
- Patient education sessions on disease management
- Population health monitoring across patient panels
- Proactive outreach for preventive care appointments
- Medication adherence tracking through regular contact
Staff roles expand beyond administrative tasks. Nurses conduct wellness checks. Care coordinators manage patient outreach. Data analysts track quality metrics. These workflow changes require additional training and resources.
How Technology Requirements Increase Under Value-Based Care
Value-based care requires a strong technology foundation. Providers need systems that track patient outcomes, measure quality metrics, and coordinate care across multiple providers and settings. A digital health platform becomes necessary for managing value-based contracts effectively.
Essential Technology Investments
Providers must invest in comprehensive technology solutions:
- Electronic health records with care coordination features
- Population health management dashboards
- Patient engagement tools for remote monitoring
- Analytics platforms for quality metric tracking
- Interoperability solutions for data exchange
These technology upgrades often involve significant upfront costs. Small practices have difficulties in paying for full systems. Providers can, however, manage quality metrics and care coordination.
What Financial Risks Providers Assume
In value-based care, financial risk shifts from payers to providers. Providers become accountable for patient health outcomes and total cost of care, including services they don't directly deliver. This accountability creates new financial pressures and requires careful population management.
Understanding Risk-Based Contracts
Providers accept responsibility for managing patient populations within predetermined budgets. Hospital readmission penalties reduce overall compensation. Emergency department overutilization impacts quality scores. Specialist referrals and diagnostic testing count against cost targets.
Additional financial risks include:
- Preventable complications trigger financial penalties
- Patient non-compliance affects outcome measurements
- Chronic disease progression reduces quality scores
- Care coordination failures lead to costly interventions
Providers need to balance quality improvement with cost control. This involves proper patient selection, vigorous coordination of care, and active disease prevention to avoid costly complications.
How Patient Relationships Transform
The difference between value-based care vs fee-for-service is the one that transforms the provider-patient relationships fundamentally. Providers are partners in patient health management as opposed to service deliverers of acute problems. This model of collaboration can be characterized by constant interaction and joint decision-making.
New Communication Patterns
Providers stay in regular contact with patients between visits. Communication deals with prevention and early intervention. Active outreach is the provision of preventative visits to patients. Monitoring of medication adherence is done via phone calls. Vital sign monitoring. Remote monitoring aids in the management of patients with chronic diseases.
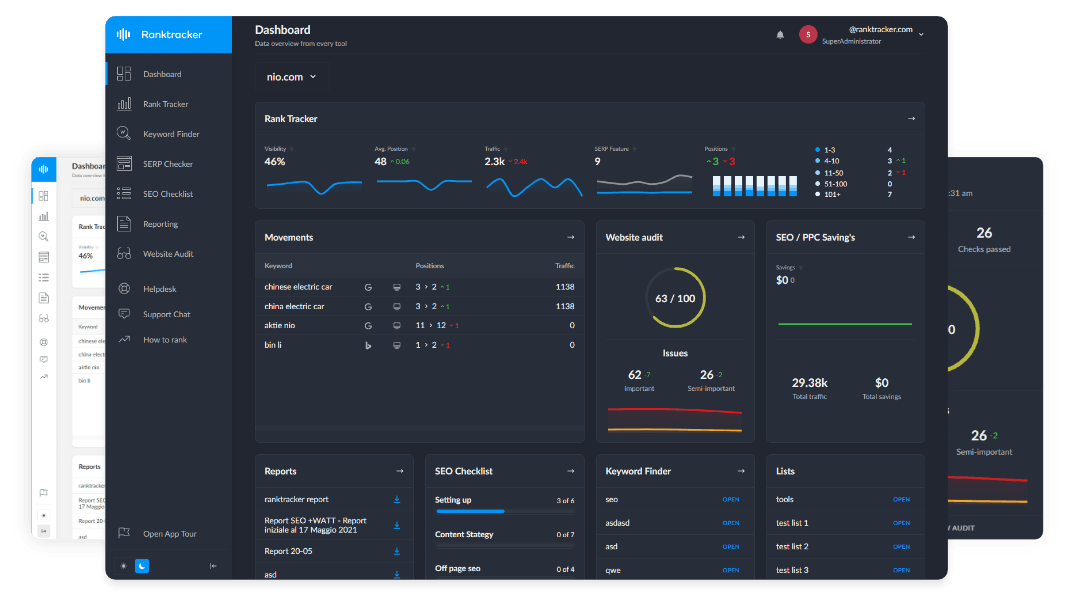
The All-in-One Platform for Effective SEO
Behind every successful business is a strong SEO campaign. But with countless optimization tools and techniques out there to choose from, it can be hard to know where to start. Well, fear no more, cause I've got just the thing to help. Presenting the Ranktracker all-in-one platform for effective SEO
We have finally opened registration to Ranktracker absolutely free!
Create a free accountOr Sign in using your credentials
Lifestyle changes are dealt with in health coaching sessions. Care plan discussions entail patient preferences and goals. Such experiences demand that providers acquire enhanced skills in interacting with patients. Clinical competencies like motivational interviewing and shared decision-making are necessary.
Why Care Coordination Becomes Essential
Value-based care makes primary care providers accountable for patient outcomes across all care settings. The providers need to align with specialists, hospitals, rehab centers, and home health organizations to control the overall cost and quality. Good coordination keeps up with loopholes that cause complexities.
Building Effective Care Networks
Successful providers establish formal relationships with other healthcare entities. Preferred specialist networks enable efficient referrals. Hospital partnerships improve discharge planning. Home health agencies support post-acute care needs.
Care coordination also requires:
- Pharmacy collaborations for medication management
- Community organizations for social determinants support
- Real-time information sharing across care settings
- Standardized transition protocols between providers
Care coordinators track patients across these settings. They ensure test results reach appropriate providers. Medications get reconciled after hospital stays. Follow-up appointments occur on schedule.
What Staffing Changes Providers Need
Value-based care introduces new roles beyond traditional clinical and administrative staff. The care coordinators, data analysts, patient navigators, and quality improvement specialists are hired by care providers to facilitate value-based operations. These additions increase practice overhead but become necessary for success.
New Team Members and Their Roles
The care coordinators involve patient outreach and follow-ups. The data analysts monitor the quality indicators and areas of improvement. Patient navigators assist patients in getting community resources. Workflow enhancement designs are developed by quality improvement specialists. Behavioral health specialists address mental health needs affecting chronic disease management.
These additions increase practice overhead costs. Providers must generate sufficient value-based incentive payments to cover expanded staffing while maintaining financial viability during the transition period.
How Preventive Care Becomes Financially Viable
In the case of fee-for-service, preventive care will produce only a small amount of revenue. Value-based care financially rewards prevention, reducing future complications and hospitalizations that hurt quality scores. Activities that previously appeared to be financially unsustainable, like prevention activities, become strategic priorities.
Prevention Activities That Drive Value
The risk to health is discovered early with annual wellness visits. Acute exacerbation is prevented by chronic disease management. Preventable illness is minimized by immunization programs. Screening for cancer identifies it at curable stages. Lifestyle counseling works at the cause level of chronic disorders.
The providers spend resources to maintain the health of the patient, instead of responding to the occurrence of sickness. This preventive strategy is better in terms of enhancing results, including minimizing the total healthcare expenditure.
Why Data Analytics Capabilities Matter
The value-based contracts demand that the providers show quality performance using data. To payers, providers must have analytics to determine high-risk patients, intervention effectiveness, and quality reporting. Analytics drive data-informed decisions that improve care quality.
Critical Analytics Functions
Risk stratification helps to identify those patients who require intensive care. Gap-in-care reports indicate the absence of preventive services. The quality measure dashboard is a tracking measure of performance. Cost analysis will indicate the possibilities for improvement of efficiency. Outcome trending shows that interventions are effective.
Providers lacking strong analytics capabilities will struggle to secure value-based contracts. They are not able to find the areas of improvement and show quality performance in order to obtain incentive payments.
Takeaway
The shift from Fee-for-Service to Value-Based Care represents a major change in how providers deliver care and receive compensation. Success requires updating workflows, investing in technology, expanding care teams, and building new coordination and analytics capabilities. Providers who adopt these changes effectively can thrive long-term in value-based payment models, where patient outcomes take priority over service volume.
Persivia offers a complete solution to simplify this transition. Population health management, quality metric monitoring, care coordination, and patient engagement are all integrated in Persivia CareSpace®. Providers gain real-time insights into patient risk, quality outcomes, and gaps in care. The platform connects clinical teams, automates outreach, and generates reports for payers. Move beyond disconnected systems and manual tracking that waste resources and slow progress.
FAQs
Does value-based care reduce provider income?
The All-in-One Platform for Effective SEO
Behind every successful business is a strong SEO campaign. But with countless optimization tools and techniques out there to choose from, it can be hard to know where to start. Well, fear no more, cause I've got just the thing to help. Presenting the Ranktracker all-in-one platform for effective SEO
We have finally opened registration to Ranktracker absolutely free!
Create a free accountOr Sign in using your credentials
No, value-based care can increase provider income through quality bonuses and shared savings payments. Providers who meet quality benchmarks and manage costs effectively earn incentive payments beyond fee-for-service rates. However, providers failing to meet performance targets face reduced compensation through penalties and withholds.
Can small practices succeed in value-based care?
Yes, small practices succeed in value-based care by joining accountable care organizations or clinically integrated networks that provide shared infrastructure. These arrangements give small practices access to care coordination resources, analytics platforms, and quality reporting tools they cannot afford independently. Collaboration helps small providers compete effectively.
How long does transitioning to value-based care take?
No, full transition to value-based care typically requires three to five years. Providers need time to implement new technology, train staff on revised workflows, establish care coordination processes, and demonstrate sustained quality performance. Most payers offer phased approaches that gradually increase risk levels as providers build capabilities.
The All-in-One Platform for Effective SEO
Behind every successful business is a strong SEO campaign. But with countless optimization tools and techniques out there to choose from, it can be hard to know where to start. Well, fear no more, cause I've got just the thing to help. Presenting the Ranktracker all-in-one platform for effective SEO
We have finally opened registration to Ranktracker absolutely free!
Create a free accountOr Sign in using your credentials
Do patients prefer value-based care over fee-for-service?
Yes, patients report higher satisfaction with value-based care due to increased provider accessibility, better care coordination, and a focus on prevention. Patients appreciate proactive outreach, longer appointment times, and coordinated care across providers. However, patient preferences vary based on health status and care needs.
Are fee-for-service models disappearing completely?
No, fee-for-service models continue alongside value-based arrangements in hybrid payment structures. Most providers maintain mixed payer panels with both payment models during the extended transition period. Complete elimination of fee-for-service remains unlikely, though value-based models represent growing payment portions for most providers.